Sara F. Morris, MAT, MPH, RD, is a research assistant in the Department of Nutrition at the University of North Carolina in Chapel Hill. Judith Wylie-Rosett, EdD, RD, is a professor and head of the Division of Behavioral and Nutritional Research in the Department of Epidemiology and Population Health at the Albert Einstein College of Medicine in Bronx, N.Y.
Clin Diabetes 2010;28(1):12–18Sara F. Morris , Judith Wylie-Rosett; Medical Nutrition Therapy: A Key to Diabetes Management and Prevention. Clin Diabetes 1 January 2010; 28 (1): 12–18. https://doi.org/10.2337/diaclin.28.1.12
Download citation file:
toolbar searchBecause of the direct correlation between diet and diabetes management, medical nutrition therapy (MNT) provided by a registered dietitian is a key complement to traditional medical interventions in diabetes treatment. This article describes MNT, summarizes evidence for the effectiveness of MNT in preventing and treating diabetes, and provides physicians with information about how to refer patients for MNT.
The link between diabetes and diet has been well documented, as has the importance of diet in conjunction with medical interventions for diabetes. Patients often look to their primary care physicians for advice about general diabetes care, including diet, but survey studies have revealed that doctors feel uncomfortable advising patients on the sensitive issues of weight loss and diet. 1 Research is increasingly demonstrating that medical nutrition therapy (MNT), administered by a registered dietitian (RD) or nutrition professional, is a key component of diabetes management and a complement to treatment of diabetes by physicians.
The American Diabetes Association (ADA) 2009 clinical practice recommendations state that “individuals who have pre-diabetes or diabetes should receive individualized MNT as needed to achieve treatment goals, preferably provided by a registered dietitian familiar with the components of diabetes MNT.” 2 Furthermore, the ADA's position statement titled “Nutrition Recommendations and Interventions for Diabetes” emphasizes the importance of MNT in preventing diabetes, managing existing diabetes, and preventing and slowing the onset of diabetes-related complications. 3 The integration of MNT into diabetes care has the potential to improve patients' diabetes management and to lessen the burden on physicians to provide nutrition information.
MNT is defined as “nutritional diagnostic, therapy, and counseling services for the purpose of disease management, which are furnished by a registered dietitian or nutrition professional.” 4 The American Dietetic Association, the professional organization of RDs, defines the nutrition counseling component of MNT as “a supportive process to set priorities, establish goals, and create individualized action plans which acknowledge and foster responsibility for self-care.” 5
In general, MNT consists of multiple, one-on-one sessions between an RD and a patient, in which the RD performs the nutrition assessment, diagnosis, counseling, and other therapy services according to the American Dietetic Association's “MNT Evidence-Based Guide for Practice/Nutrition Protocol” or according to the best available current evidence in the nutrition community. 5 After an RD receives a referral from a physician, the framework of counseling is standardized and documented as part of the American Dietetic Association's Nutrition Care Process (nutrition assessment, nutrition diagnosis, nutrition intervention, nutrition monitoring, and evaluation). 6
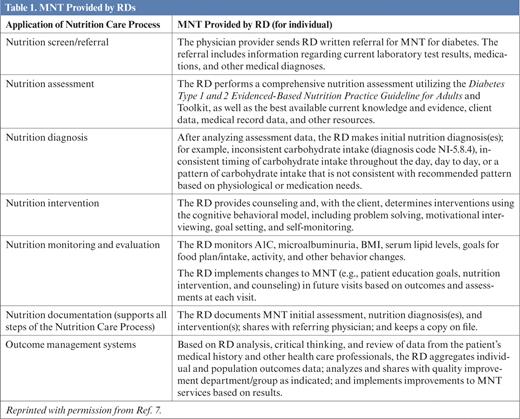
The components of MNT provided by an RD, according to the Nutrition Care Process for any nutrition-related disease (not just diabetes), are outlined in Table 1. 7 Initially, the dietitian performs a nutrition assessment of the patient's dietary patterns. This assessment, in conjunction with information about laboratory testing, medications, and any other conditions that the RD would have received with the physician referral, allows the RD to evaluate such factors as the patient's macronutrient needs versus intake, the consistency of meals, the amount and consistency of carbohydrate intake, and the general quality of the patient's diet. The RD can then issue a coded, standardized nutrition diagnosis and tailor future individual counseling to help the patient meet goals related to the diagnosis and nutrition needs.
As an example, after reviewing a patient's physician referral information and dietary patterns, an RD might issue the following diagnostic statement: “Inconsistent carbohydrate intake related to inadequate meal planning as evidenced by meals and snacks containing a range from 0 to 150 g of carbohydrates on a daily basis.” The nutrition intervention for this diagnostic statement might consist of the RD teaching the patient to plan meals and carbohydrate intake using the diabetes plate model or the carbohydrate exchange methods, helping the patient set goals related to consistent intake, and then using motivational interviewing or problem solving to address any barriers the patient has to meeting nutritional goals. 8,9
MNT Provided by RDs
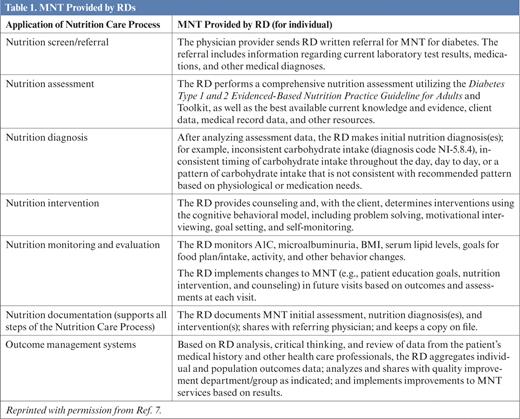
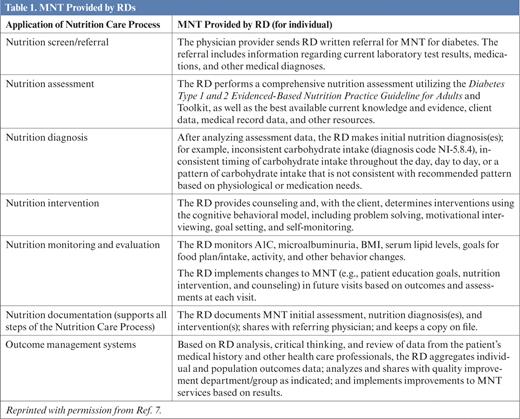
As part of nutrition monitoring and evaluation, the RD monitors biochemical factors such as A1C and serum lipid levels, as well as lifestyle factors such as dietary intake. Depending on how many sessions the RD has with the patient, these factors are used to evaluate the effectiveness of interventions in meeting goals. Diagnoses and interventions might then be revised based on nutrition-related outcomes. Therefore, MNT for nutrition-related disorders such as diabetes is not necessarily a linear process. Counseling in MNT is individualized and tailored to a patient's clinical and lifestyle needs.
MNT is not synonymous with diabetes self-management training (DSMT). DSMT is an education and training program that helps patients manage their diabetes, whereas MNT consists of more individualized diagnosis, therapy, and counseling related to nutrition. 7
According to the American Dietetic Association's 2009 White Paper on Nutrition Services that distinguishes between the delivery of DSMT and MNT services, the DSMT curriculum that is accredited by Medicare consists of 1 hour of individualized assessment and 9 hours of group classes. 7 One of the content areas outlined in the DSMT curriculum is “incorporating nutritional management into lifestyle,” but others are less nutrition related, such as “using medications safely and for maximum therapeutic effectiveness.” 7
MNT for patients with diabetes is administered in several sessions with an RD, who provides “more intensive nutrition counseling and a therapy regimen that relies heavily on follow-up and feedback to assist patients with changing their behavior(s) over time.” 7 Furthermore, although MNT for diabetes patients can be administered only by a licensed/certified RD or nutrition professional, DSMT can be administered by a registered nurse, dietitian, or pharmacist. 7
Sometimes it may be most helpful for patients to receive DSMT first, followed by MNT. Other patients may receive DSMT and MNT simultaneously. Professional organizations such as the ADA, the American Dietetic Association, and the Centers for Medicare and& Medicaid Services recognize both the distinctions between DSMT and MNT and the possibility that the two programs can complement each other.
Research has shown MNT to be effective for the treatment of both type 1 and type 2 diabetes. The American Dietetic Association reviewed 18 studies that involved the provision of MNT by an RD as part of treatment for either type 1 or type 2 diabetes. Of these, all 8 of the randomized controlled trials reviewed demonstrated a positive effect of MNT in diabetes management, measured by improvement in A1C levels. 10 Based on this review, the American Dietetic Association reports strong support for the effectiveness of MNT provided by RDs in the management of type 1 and type 2 diabetes and suggests that MNT has the greatest potential for impact when diabetes is first diagnosed. 10
Summary of Evidence for Nutrition Therapy in Diabetes 11-26
Several studies in which MNT was included in diabetes treatment interventions that successfully affected metabolic and behavioral outcomes are summarized in Table 2, adapted from Pastors et al. 11-26 The studies varied in design and length (from 3 months to 9 years), and some were conducted before MNT for diabetes was as well defined as it is today. However, all studies listed implemented at least one study group that received individual counseling from an RD, with number of sessions ranging from two total sessions to monthly sessions for 6 months or more. These studies reported improvements in A1C ranging from 0.9 to 1.9% for groups receiving MNT and generally reported a greater improvement in A1C when compared to study groups that received less intensive or basic nutrition education. 11 In general, Pastors et al. summarize that “randomized controlled nutrition therapy outcome studies have documented decreases in [A1C] of ~1% in newly diagnosed type 1 diabetes, 2% in newly diagnosed type 2 diabetes, and 1% in type 2 diabetes with an average duration of 4 years.” 11
MNT has also been shown to be effective in the prevention of type 2 diabetes. Although the onset of type 1 diabetes is not considered to be preventable, the onset of type 2 diabetes can be delayed or prevented with lifestyle modifications, including changes to diet. Based on its review of seven studies that implemented nutrition therapy and 16 studies that implemented intensive lifestyle interventions including nutrition therapy, the American Dietetic Association concluded that MNT is “effective at reducing the incidence of type 2 diabetes.” 10
The same review concluded that pharmacotherapy is also effective at reducing incidence of type 2 diabetes, but stated that in all but one of seven studies reviewed, lifestyle interventions were more effective than pharmacotherapy at reducing incidence. 10 Regarding pharmacotherapy, it should be noted that although the ADA clinical practice recommendations do endorse the use of medications to treat certain complications of diabetes, they also endorse MNT and lifestyle changes as alternatives and complements to pharmacotherapy. 2
A notable prevention study is the Diabetes Prevention Program, reported in 2002. 7 In this randomized, controlled trial of 1,079 participants aged 25-84 years, a 58% reduction in incidence of diabetes over 3 years was reported in subjects treated with an intensive lifestyle intervention that included MNT.
Based on the results of this prevention intervention, the Look AHEAD (Action for Health in Diabetes) study is currently underway to test the effects of similar lifestyle interventions in the treatment of 5,145 men and women who have already been diagnosed with type 2 diabetes. 8 Although this trial is planned to extend for 11.5 years, the researchers' recently published 1-year results reported that the intensive lifestyle intervention group lost 8.6% of initial weight compared to 0.7% in the control group. 28 The intensive lifestyle intervention included comprehensive diet counseling from an RD, whereas the control group received basic, or “usual,” care for diabetes. The experimental group also had significantly greater decreases in A1C, systolic and diastolic blood pressure, and triglyceride levels in the first year, compared to the control group. 28
The body of evidence pointing to the effectiveness of MNT in treating, and now preventing, adult type 2 diabetes continues to grow. However, research on the effectiveness of MNT for diabetes in children and adolescents is still limited. The Diabetes Control and Complications Trial, reported in 1993, did include subjects aged 13-39 years. 29 This randomized, controlled trial showed 34-76% reductions in complications of type 1 diabetes in the study group, which received both intensive insulin therapy and monthly clinic visits with an RD.
It is only within the past decade that the prevalence of type 2 diabetes among children and adolescents has been recognized, but studies currently underway are demonstrating that the incidence and prevalence of type 2 diabetes are increasing. 30,31 Therefore, there is a need for research to identify the most effective interventions to address the prevention and treatment of type 2 diabetes in children and adolescents. Even so, based on the existing evidence pertaining to adults with type 2 diabetes, the contribution of MNT to the prevention and treatment of this disease in children is promising.
Although the ADA and the American Dietetic Association are in agreement that patients with pre-diabetes and diagnosed diabetes should be referred for MNT, many primary care physicians are unsure of how to go about making these referrals.
Medicare generally serves as the standard for other third-party payers, so many private and state insurance plans also cover MNT for diabetes management. In fact, as of 2009, 46 states and the District of Columbia have legislation in place that requires insurance coverage for diabetes management, although the breadth of coverage offered varies greatly from state to state. 33
However, although Medicare and other third-party payers cover diabetes screening for patients who have been diagnosed with pre-diabetes, Medicare does not currently cover MNT for patients with pre-diabetes. 34 The Diabetes Prevention Program study has done much to underscore the effectiveness and cost-effectiveness of lifestyle interventions, including MNT, in preventing or delaying the onset of type 2 diabetes. 27,35 In this time of insurance reform, it is possible that coverage for MNT for pre-diabetes, considered to be a preventive service, will become more widespread.
It is important to note that Medicare coverage of MNT for people with diabetes requires a physician referral. According to Medicare MNT legislation, patients with a physician referral can receive 3 hours of individual counseling with an RD during the first year of treatment and 2 hours of counseling each year after that. 4,5,7 Medicare also covers DSMT in addition to MNT without decreasing the benefit of either. 7
Patients who are not covered under Medicare insurance should still be referred for MNT because many private insurers will cover MNT for diabetes and other conditions. 36 To ensure that patients will be eligible to receive MNT through third-party coverage, the American Dietetic Association suggests the following guidelines for physicians: 36
To assist patients in locating an RD, physicians can access the “Find a Nutrition Professional” section of the American Dietetic Association's Web site, www.eatright.org.
Some nutrition professionals hold the certified diabetes educator (CDE) credential in addition to the RD credential. CDEs are defined as “health care professionals who have defined roles as diabetes educators, not … those who may perform some diabetes-related functions as part of or in the course of other usual and customary occupational duties.” 37 CDEs may be nurses, doctors, dietitians, or other health care providers. Whatever their discipline, they must have 2 full years of professional practice experience, perform 1,000 hours of diabetes self-management education (DSME), and take an accreditation examination to earn the CDE credential.
DSME is synonymous with DSMT. Therefore, the scope of diabetes self-management education provided by CDEs includes not only a nutrition education component, but also education and training in the effects of diabetesrelated medicines, self-monitoring of blood glucose, and administering insulin. 6,37
The difference between DSMT/DSME and MNT has been explained; the treatments are complementary but not identical in scope. Therefore, although a health care professional who is a CDE may be able to advise patients regarding some aspects of diabetes nutrition, only an RD can provide intensive MNT.
It is arguably ideal to refer patients who need diabetes MNT to RDs who are also CDEs, because these individuals would be experts in the nutrition aspect of diabetes and trained to educate patients in some non-nutrition aspects of diabetes management. However, the professional to whom patients are referred for MNT must, at the minimum, hold the RD credential.
MNT is an effective and increasingly affordable method to prevent type 2 diabetes and to treat both type 1 and type 2 diabetes. It is endorsed for the treatment of diabetes by the Institute of Medicine, the American Dietetic Association, and the ADA and is covered by Medicare. The provision of MNT by RDs, who are experts in offering individualized nutrition counseling, will improve the quality of counseling offered to patients and alleviate the burden on physicians to provide nutrition education. Primary care physicians should refer patients with symptoms of pre-diabetes and diabetes for MNT services, to be provided by an RD, to ensure the best care for their patients.